What Causes Herniated Cervical Discs?
Herniated cervical discs are likely a consequence of progressive wear and tear on the spinal column, leading to weakening of the annulus fibrosus and subsequent disc herniations. Occasionally herniated discs can be associated with an acute traumatic event. Most patients with herniated cervical discs experience symptoms upon awaking in the morning without associated trauma or mechanical stress.
How Are Herniated Cervical Discs Discovered?
When a cervical disc herniates it potentially can compress a nerve root and sometimes even the spinal cord. When a nerve root is compressed, the patient may experience neck pain that radiates into the shoulder and/or arm. If the compression of the nerve root is severe a patient may experience weakness in the associated muscle groups.
When a disc herniation compresses the spinal cord it can result in a different constellation of symptoms called cervical myelopathy. With cervical myelopathy a patient frequently complains of difficulty using the hands when performing fine motor tasks (such as writing with a pen or buttoning a shirt). This hand clumsiness is sometimes associated with numbness of the fingertips. Also compression of the cervical spinal cord can result in difficulty walking with frequent stumbling and falls.
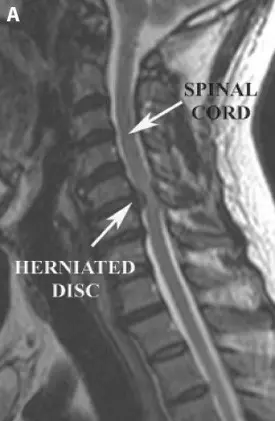
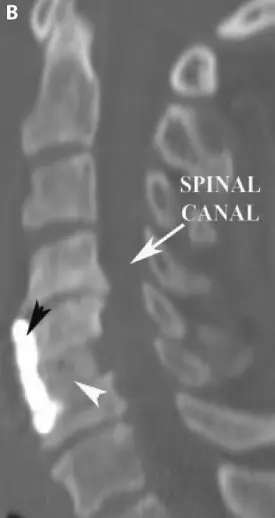
When a herniated disc is suspected, diagnostic tests like an MRI (Magnetic Resonance Imaging) and/or a CT (Computed Tomography) scan can provide the anatomic detail to confirm the diagnosis.
How Can Cervical Herniated Discs Be Treated?
Many of the symptoms associated with herniated cervical discs resolve without surgery. Surgical intervention is typically reserved for severe pain that does not respond to medical therapy, severe weakness, and myelopathic symptoms arising from spinal cord compression. Surgical options include single and multilevel anterior cervical discectomy and fusion (ACDF), removal of a cervical vertebral body (corpectomy), and cervical foraminotomy and discectomy. Some patients with single level cervical disc disease may even be candidates for placement of an artificial cervical disc. The surgical approach is determined on in individual basis, taking into consideration both the patient’s anatomy and symptomatology.
A) Pre-operative sagittal T2 weighted MRI demonstrating a herniated cervical disc compressing the spinal cord
B) Post-operative sagittal CT scan of the cervical spine demonstrating an anterior cervical discectomy and fusion (ACDF). A bone graft is placed (white arrowhead) in the empty disc space and a plate (black arrowhead) is placed on the front of the spine to hold the bone graft in place