What Causes Trigeminal Neuralgia?
Trigeminal neuralgia, in most cases, is caused when a blood vessel compresses the trigeminal nerve as it exits the brain stem. Rarely tumors, cysts, or vascular malformations can compress the trigeminal nerve as it exits the brain stem, causing lancinating facial pain. Multiple sclerosis affecting the brain stem can also cause trigeminal neuralgia.
How Is Trigeminal Neuralgia Diagnosed?
The patient’s presenting symptoms are unique to the disease and frequently are enough to definitively diagnose trigeminal neuralgia. An MRI of the brain and brainstem is often obtained to ensure that a tumor, cyst, vascular malformation, or multiple sclerosis is not the cause of the symptoms. In evaluating a patient for trigeminal neuralgia, other potential sources of facial pain must be excluded, such as: herpes zoster, dental disease, infections or tumors of the eye and orbit and temporal arteritis.
How Is Trigeminal Neuralgia Treated?
The initial treatment of trigeminal neuralgia is with medication such as carbamazapine, clonazepam or amitriptyline. Up to 70 percent of patients experience symptomatic relief with medication alone. When medication fails to provide adequate relief, or when a patient begins to experience severe side-effects from the medication surgical option need to be considered.
The primary surgical treatment for trigeminal neuralgia involves exposing the facial nerve as it exits the brainstem and identifying the blood vessel that is compressing the nerve. This blood vessel is then separated from the nerve using a piece of Teflon felt. This procedure, called a microvascular decompression (MVD), may result in pain relief for a period of 10 years or more in 70 percent of patients.
For patients who either are not healthy enough for surgery or who do not wish to undergo a surgery may opt for a percutanious glycerol rhizotomy unsing local anesthesia. A glycerol rhizotomy involves inserting a needle though the skin, into the opening of the skull (foramen ovale) where the trigeminal ganglion is located. X-ray guidance is used to confirm proper location of the needle. Glycerol is then injected resulting in an injury to the nerve fibers which transmit the pain sensation. Unfortunately the results are not as good as with an MVD, and some patients may experience persistent post procedural facial numbness.
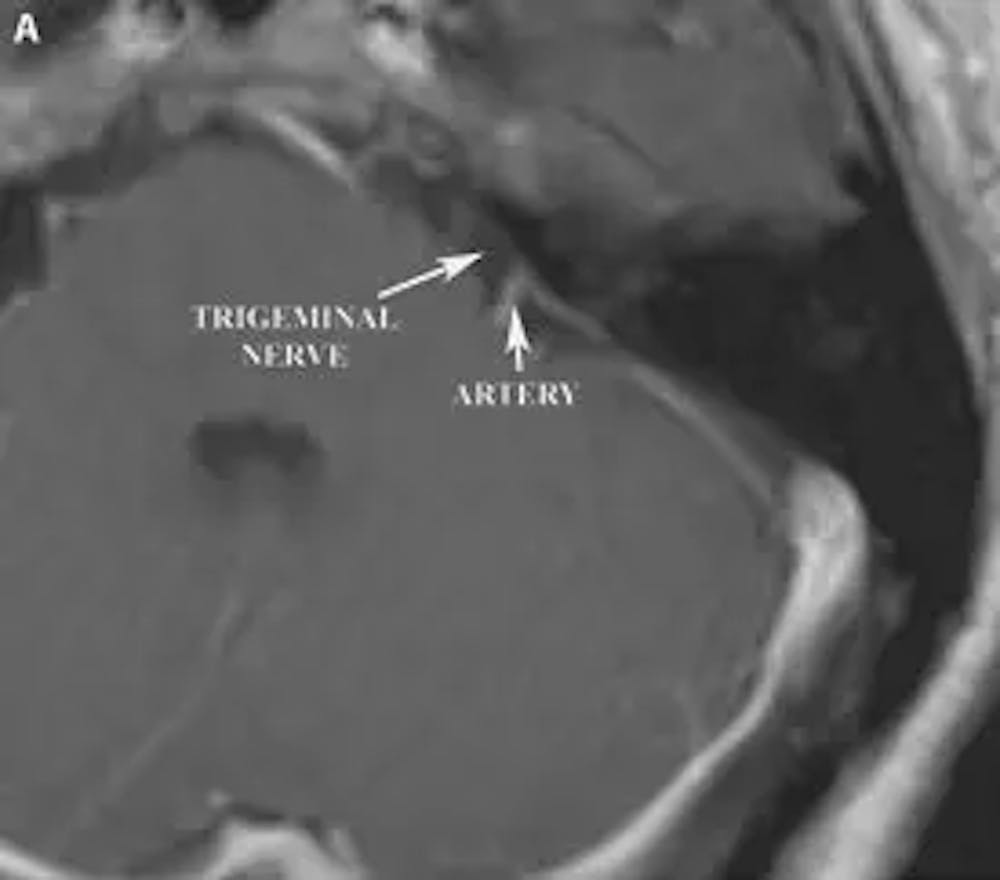
A) Pre-operative axial T1 weighted MRI of the brain with contrast demonstrating proximity of a loop of the superior cerebellar artery to the trigeminal nerve.
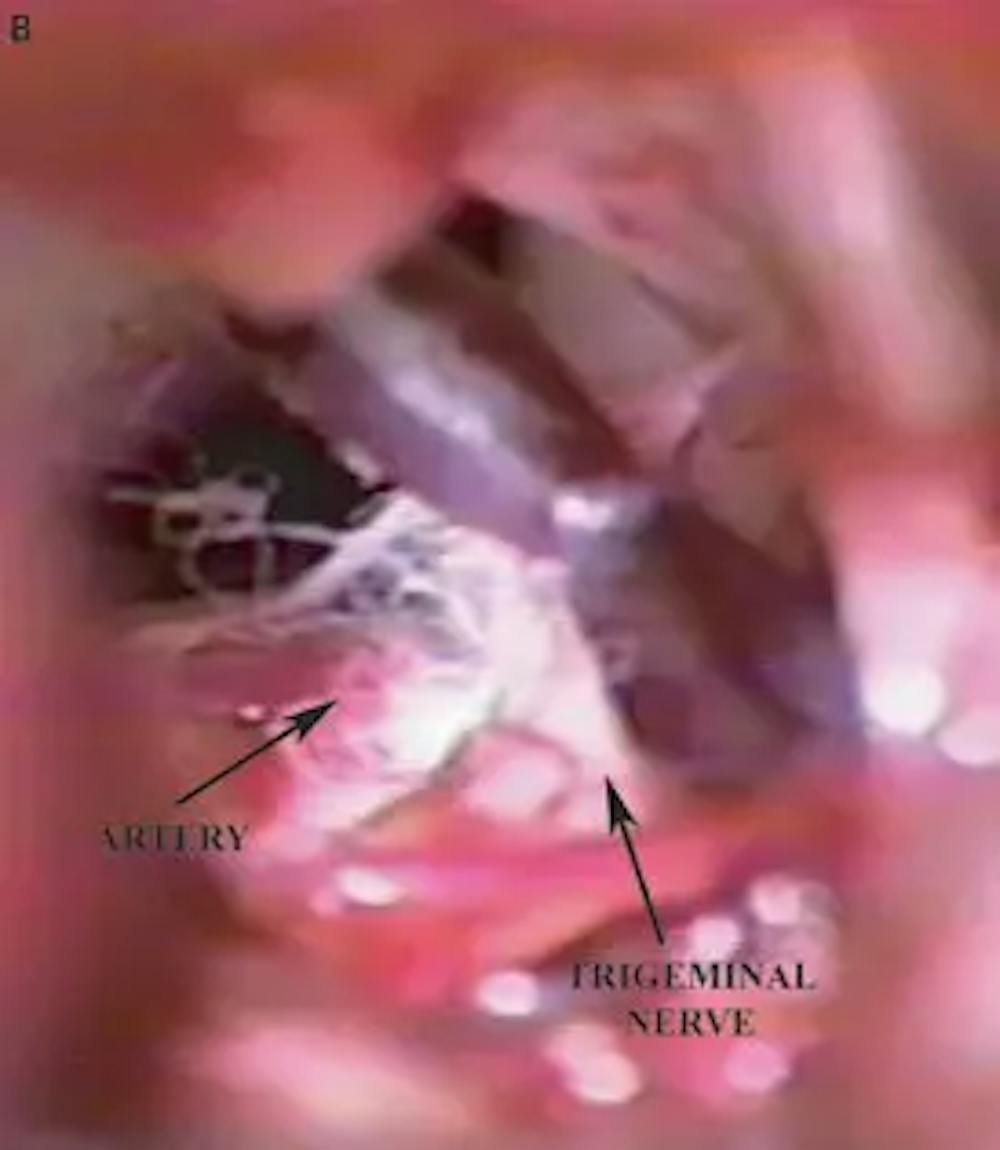
B) Intra-operative photograph demonstrating a loop of the superior cerebellar artery contacting the trigeminal nerve.

